Lens Replacement Surgery
What is Lens Replacement Surgery (LRS) or Refractive Lens Exchange (RLE)?
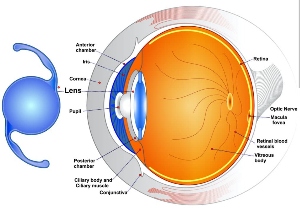
Behind the pupil in the eye is a lens that is used for fine focusing. With advancing age, the lens becomes harder and stops changing shape, which results in the need for reading glasses. With time and further hardening the same lens becomes cloudy and eventually affects the ability to see, this is then called a cataract. Lens replacement is similar to cataract surgery in that the dysfunctional lens (and often clear lens) is removed and replaced with a sophisticated high performance intraocular lens implant measured specifically to suit each eye.
At Centre for Sight, a laser (rather than a manual technique) is used to assist the process in Lens Replacement / Exchange and is performed in this manner in 100% of cases and at no additional cost.
The aim of the operating surgeon is to provide spectacle independence and to accomplish this a high level of accuracy is required. The procedure is achieved through an incision measuring just 1.8mm across, with the most critical portions of the surgery are performed by laser ensuring repeatability and increased safety with less time spent in the eye.
Suitability for Lens Replacement Surgery
Generally, those over the age of 50 with any level of hyperopia (farsighted), and 55 with any level of myopia (shortsighted) and/or astigmatism, can be suitable for Lens Replacement Surgery. Those who have cataracts are often suitable for high performance trifocal lenses, which provide a full range of focus.
To be suitable for multifocal lenses, good eye health is essential – with no identified problems that may affect lens performance. Those with macular degeneration or visual field loss from glaucoma, for instance, will not be suitable for multifocal (trifocal) lenses. Additionally those with diabetes are not suitable for lens replacement and if they have cataracts a monofocal or advanced monofocal lens is a better option.
Safety is paramount
At Centre for Sight, we are very selective about those who are eligible. Safety is our number one priority and we make our decisions based on scientific evidence, delaying (or first treating any underlying condition where appropriate) and even declining those who might be at increased risk of complications during lens replacement / exchange surgery.
Special characteristics
The natural crystalline lens in the eye becomes harder with advancing age and in turn fails to change shape adequately to alter focus for near vision. A change in shape is necessary when looking at near objects e.g. reading a book or iPad.
The natural lens functions inadequately and the condition is termed by some as “Dysfunctional Lens Syndrome” (DLS). The crystalline lens becomes progressively harder and in turn near focus deteriorates further with advancing age. Reading glasses which become progressively stronger are needed to be able to see. This condition is also called Presbyopia. There are several options available to surgically correct Presbyopia using intraocular lenses and these are outlined below.
What are the different types of lens surgery?
Trifocal Multifocal Lens
This is the most common type of lens used for full vision correction at Centre for Sight (since 2011) with more than 90% of patients undergoing lens surgery with this type of lens implant. The advantage of this lens is it reliably provides correction of distance, intermediate and near vision, in other words a full depth of focus, eliminating or reducing the need for glasses.
Suitability for the lens implant is determined at consultation when numerous tests including the optical properties of the cornea and tear film are evaluated. To work well, these high performance lenses require a cornea with good optical properties as well as a surface free of dryness and no streaky tear film. Patients must understand the concept of adaptation or neuro-adaptation which involves the brain becoming accustomed to the new sophisticated optical system to pick up and interpret useful information.
The lens has microscopic rings which provide near and intermediate vision and as a consequence patients may well experience transient halos that disappear with adaptation. Visual ability also improves with time from gradual neuro-adaptation.
Trifocal – PiggyBack Lens
For those who have already had lens replacement / exchange or cataract surgery and were not lucky enough to have a trifocal lens, there is an option of adding in a trifocal lens implant on top of the existing lens. This is also available at primary cataract surgery. For instance if someone has Glaucoma or macular degeneration, they may in time have a problem with the presence of a trifocal implant and may require removal. As an add-on lens placed on top of a monofocal, the lens can easily be removed from the eye. It is however reassuring that multifocal lenses have been in use at Centre for Sight since 2002 and to date no lenses have required removal for glaucoma or macular degeneration.
Trifocal Toric Lens
In those who have a significant amount of astigmatism, trifocal lenses with inbuilt astigmatism can be used to correct vision at all distances (Full range of Focus). These multifocal / trifocal lenses are specially ordered based on specific measures taken at consultation. In terms of performance, these are otherwise identical to Trifocal lenses discussed above. About 30% of patients at Centre for Sight require toric lenses.
Increased Range of Focus Lens (IROF)
This type of lens referred by some as an EDOF (Extended Depth of Focus) lens is one that reliably provides distance and intermediate vision. To improve the range of focus further, the non-dominant eye is adjusted so that this becomes very slightly short-sighted, and this provides most patients with near vision. The lens is considered in those who are unsuitable for Trifocals (a full range of focus lens). The type of IROF lens used at Centre for Sight has some advantages in that there are no significant halos, however some like with the trifocals still require a period of adaptation to obtain optimum use of the lenses.
Monofocal Lens
The single focus lens is used in conventional cataract surgery for instance in the NHS and vision is often geared for distance only which means recipients will in all probability require glasses for intermediate and near vision. Monovision is where the lens power can be adjusted to provide near vision in one eye (usually the non-dominant eye) and distance correction in the dominant eye. This provides good depth of focus between the two eyes and is very useful. For many the disparity between the two eyes is a nuisance and not everyone is able to get used to this option of Monovision sometimes also called Blended Vision.
Monofocal Plus
This lens implant provides a greater range of focus than a standard monofocal implant. It is useful as an alternative in those not suitable for trifocals but wish to have increased range of focus. Distance and intermediate vision are often good however for near vision glasses are still required. A micro-monovision arrangement sometimes is used with one eye made very slightly myopic providing improved near vision with both eyes open.
Extended Depth of Focus (EDOF) Lens
Poorly termed, this lens like a Monofocal Plus increases the range of focus but with slightly better performance. The term EDOF comes from photography and Centre for Sight doctors are involved in devising new international terminology to address this confusion. This article published in Cataract and Refractive Surgery Today- Europe “Let’s speak Lens peak” authored by medical director Sheraz Daya provides some insight.
Toric Lens
This is a lens that has astigmatism built in to the implant and used in those with astigmatism on their cornea of 1.25D and above. For those with less astigmatism, limbal relaxing incisions are at Centre for Sight performed using the laser employed in Lens replacement surgery. Toric lenses have to be specially ordered and sometimes need to be manufactured to suit the individual eye. This may increase the lead time for surgery. Toric lenses are available in combination with both Monofocal and Trifocal lenses.
The Consultation
At Centre for Sight a thorough preoperative consultation will be conducted by the Consultant Surgeon who will carry out your procedure. The surgeon is supported by a team of highly trained technicians who perform a minimum set of investigations and measurements.
Based on initial findings, additional investigations may be required to further evaluate the eyes as necessary. During the process, ophthalmic technicians and optometrists are in constant contact with and directed by the Ophthalmic Consultant surgeon. Once this has been accomplished the patient will be seen and counselled further by the Consultant surgeon.
Tests performed at Consultation
The consultation at Centre for Sight routinely involves evaluation of vision and refraction (eye testing), contrast sensitivity, corneal mapping, a check of the overall eye aberrations and the contribution of aberrations made by the cornea and the lens within the eye.
A dry eye test (Schirmer’s test) is also performed as well as a pressure check (Tonometry) and corneal thickness evaluation (Pachymetry).
A scan of the retina and optic nerve (Ocular coherence tomography) to check the health of the back of the eye and rule out any conditions that may adversely affect the outcome of eye Lens replacement / exchange.
The eyes are dilated and a wide-field retinal scan is performed followed by an evaluation by the Consultant. During the process, if not seen already prior to consultation there will be an opportunity to watch very helpful schematic videos about the procedure, the lenses used and what to expect.
Additionally, a copy of the consent form will be provided to read in advance and may generate questions which can be answered by the Consultant. The Consultant will look through all the data provided and also perform a thorough evaluation of the front and back of each eye and consider suitability of the procedure.
Your Consultant will discuss the overall findings and outline any special considerations specific to you and your eyes and if not suitable will indicate why.
Following the consultation, you will be provided a summary of the consultation, as well as the costs of the procedure for you to consider.
The Procedure
The procedure is typically performed under drop anaesthetic. At Centre for Sight most patients opt to have intravenous sedation which involves insertion of a venous cannula and periodic injection of sedatives to keep you well relaxed. Your pupils will be dilated with a series of eye drops and possibly with a medicine pellet under your lower lid. You will also receive strong antibiotic eye drops to kill bacteria and prevent infection.
You will be brought into the operating theatre and asked to lie down on the bed attached to the laser. The surgeon looking down a microscope will attach a suction ring to the eye, which itself will be attached to the laser. You might have a sensation of slight pressure. The laser portion process takes between 1 – 2 minutes and involves making an opening in the lens capsule, and when required, fragmentation of the lens and making a corneal incision for the correction of astigmatism.
Once accomplished, the laser bed is rotated under another microscope and surgery continues. A sticky plastic drape is placed on the eye after the surrounding skin has been disinfected with an iodine preparation. An eyelid clip is used to keep the eyelids open and the surgeon will perform the remainder of the operation through an opening of 1.8 mm!
The fragmented lens is removed by a combination of suction and ultrasound, followed by lens implantation. On completion, antibiotics are instilled to prevent infection followed by the eye being patched and a protective shield placed. Treatment to the other eye is often planned within a few days to a week afterwards. For some there is an option to have both eyes treated on the same day.
Can Lens Replacement Surgery be performed on both eyes at once?
Surgery on both eyes is sometimes performed where clinically appropriate (This is called Bilateral sequential surgery). Patients suitable for surgery on both eyes are usually non-complex “middle of the road” cases. At Centre for Sight to ensure maximal safety, each eye is treated independently with different batch numbers of devices and medicines for each eye, as well as instruments that have had different sterilisation cycles.
If both eyes are treated on the same day, for practical reasons the eyes are not patched and instead goggles on an elastic band are placed to protect the eyes. Patients are advised to go home and keep their eyes closed to allow them to settle for at least 4 hours. Eye drops are also commenced on the same day and patients must be seen in consultation the following day.
Aftercare & Recovery
You will have some time to recover following surgery and when ready you will be served a light snack. You will be given a small toiletry bag containing your medications and instructions on their use. You will then be able to go home and we suggest you get plenty of rest that day.
The following day, you should take off your shield and patch. Preserve the shield in case you are instructed to use this at bedtime. Commence your drops as instructed remembering to close your eyes for 5 minutes by the clock before adding the next drop. You may have an appointment to be seen that day or a day or two later. If you are not seen the next day, someone from Centre for Sight will contact you to ensure you are making good progress.
The good news is visual recovery is typically very quick with many patients obtaining excellent vision the day following surgery. Sometimes vision is blurred for one or two days for a variety of reasons and this might be the case if the cataract was particularly hard.
A high-performance lens like a trifocal lens implant provides the ability to read without glasses. A monofocal lens corrected for distance vision often results in poor near vision easily remedied by a temporary pair of off the shelf reading glasses.
What to expect after Lens Replacement Surgery?
Adaptation (Neuro-adaptation)
When one eye is treated at a time, patients often report the following day that their vision in the treated eye is not quite as good as expected. This is often the case in those who were previously farsighted and can find that distance vision is blurred. This happens because the eye muscles which are trying to focus in the untreated eye, result in the implant being pushed forward making the patient short-sighted. For those previously shortsighted, distance vision is reported as very good, however near is initially a struggle and with adaptation improves. The brain eventually picks up the information that it needs and vision improves. With trifocal lenses, we emphasise preoperatively that it is only when BOTH eyes are treated that patients get the benefit from the lenses with no comparative reference points. The eyes see similarly and vision improves rapidly each day.
Visual side effects
Initially halos around headlights interfere with the ability to drive comfortably affects 10% of patients, but improves in all patients with time. With adaptation, the brain is able to suppress unwanted information and patients report noticing a reduction in the size of the halos over the next 6 to 12 weeks, eventually disappearing or being just a nuisance. A few patients take longer to adapt (12 to 18 months). In the worst case scenario the implant can be replaced with a monofocal lens, which will have the consequence of reducing the depth of focus and result in the need for glasses.
Dry eye
We check for dry eye before surgery and this is treated if found to be significant. Those with marked tear surface abnormalities are not suitable for multifocal lenses. The abnormal surface can affect the performance of the lenses and cause fluctuation in vision. This condition can be treated in advance and once better, patients can be considered for multifocal lenses. Dry eye after lens replacement surgery can occur as a result of a) no longer wearing glasses or contact lenses and being exposed to the elements or more commonly b) toxicity from the eye drops which are at a high concentration in order to penetrate and enter the eye. Preservatives in drops are also a contributory factor. Dry eye symptoms and effects do improve a few weeks after the course of eye drops has been completed.
Reading and intermediate vision
Trifocal lenses distribute light energy to three points of focus. The majority (60% or more is for distance and the remainder for intermediate and near. Also, some trifocals have more energy concentrated near the centre of the lens, as pupils typically constrict when one reads. However, in dim light, the pupils can dilate and thus affect reading performance, so reading menus in a dimly lit restaurant might be problematic. Using a light to illuminate the object should help. The ability to see at intermediate (computer monitors) can in some patients take time (6 to 12 weeks) and again this is to do with adaptation. The brain adapts and uses the information that is being transmitted from the retina.
Eye Lens Replacement Risks / Complications
As in all forms of surgery problems can occur during the operation or afterwards during the period of healing afterwards. Problems following Lens Replacement Surgery are fortunately rare. Common problems are easily remedied by medication or even further surgery. Serious problems are thankfully even more rare but could potentially lead to loss of vision, which can be permanent (a reduction in vision when compared to before surgery that cannot be corrected with glasses or contact lenses).
At Centre for Sight, quality standards over and above the minimal requirement by the Royal College of Ophthalmologists are collected and reported each month, which include unexpected complications during surgery, returns to the operating theatre, infections and enhancements. We are pleased to report that we have complication rates that are significantly below the national average.
Loss of vision whereby vision even with glasses or contact lenses is below the standard required for driving can occur after any eye procedure and following Laser Lens Replacement Surgery is between 1 in 500 and 1 in 1000 nationally.
The cause of this type of problem could be infection or inflammation after surgery, retinal detachment after surgery or bleeding at the time or after surgery and also posterior capsule rupture, which is where the membrane of the lens could break during surgery.
The UK rate of rupture is 1.5 to 2.0%. At Centre for Sight our rate over the last 3 years has been less than 1 in 800 (0.125%). A posterior capsule rupture may affect the ability to implant a multifocal/trifocal lens implant.
Additional Surgery
Second operations are sometimes needed and these include re-centering or repositioning a lens (for instance a Toric lens used to correct astigmatism), top-up laser surgery (1% at Centre for Sight) to correct the refraction of the eye (shortsighted, farsighted or astigmatism). Those who are shortsighted are at higher risk of retinal detachments for the first few years following Laser Lens Replacement surgery. Detached retinas are fortunately repairable by expert retinal surgeons.
Alternative procedures to Lens Replacement Surgery
Laser vision correction
Laser eye surgery procedures include LASIK (Laser in situ Keratomileusis) or Transepithelial Photorefractive Keratectomy (PRK), work by changing the shape of the cornea and therefore do not involve a lens implant.
Phakic Intraocular Lenses
These are lens implants inserted into the eye without removal of the clear natural lens.
Both the above options are better for those under the age of 50, who still have clear lenses and good quality of vision with glasses or contact lenses. Both laser vision correction and Phakic intraocular lenses are able to reliably correct one point of focus and usually distance, which means those in their mid-forties might still need to wear reading glasses afterwards. There are options for extending depth of focus and providing the ability to read and include “Monovision” or “Blended Vision” and in the case of laser eye surgery “Supracor Lasik”.
Monovision
Monovision is a technique whereby the non-dominant eye is planned for near vision and the dominant eye for distance. This means both eyes do not see equally at distance and near, however with both eyes open a good depth of focus is achievable. This is not suitable for everyone and a contact lens trial using this scenario is advised prior to undergoing the procedure. Some may already be using this method with their contact lenses.
Supracor Lasik
This is a Lasik laser eye surgery procedure where the cornea is purposefully made to be multifocal. As there is a period of adjustment and adaptation, only the non-dominant eye is treated. More information on Supracor Lasik.